- Messages
- 1
- Best answers
- 0
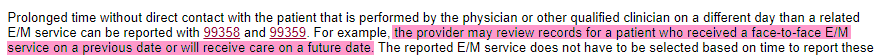
I have a provider that requires an MRI be reviewed to determine if he will take on a case. Have any of you ever billed for medical records review using CPT code 99358? Have you had successful reimbursement doing so? Would we still be reimbursed if he chose not to take the case on?